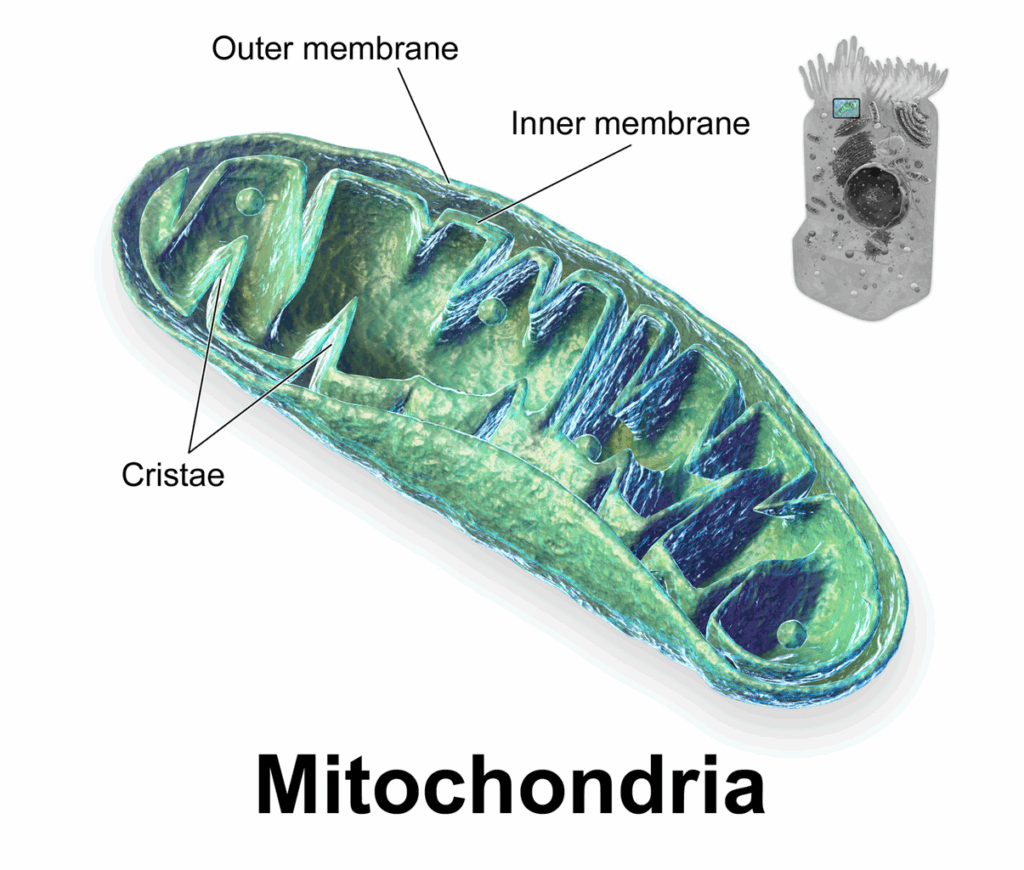
Mitochondria, often dubbed the “powerhouses of the cell,” play a central role in energy production. These tiny organelles are responsible for converting nutrients from the food we eat into adenosine triphosphate (ATP), the primary energy currency that fuels all cellular processes. Given their fundamental role in energy metabolism, it’s perhaps unsurprising that mitochondria have a significant connection to the development of obesity, a condition characterized by excessive fat accumulation resulting from an imbalance between energy intake and expenditure.
Mitochondrial Function and Energy Balance
To understand the link between mitochondria and obesity, it’s crucial to appreciate how these organelles function in maintaining energy balance. Mitochondria are the primary sites of fatty acid oxidation, a process where fats are broken down to generate ATP. They also play a key role in glucose metabolism through the citric acid cycle and oxidative phosphorylation. Efficient mitochondrial function ensures that the energy derived from food is effectively converted into usable energy, preventing its storage as excess fat.
Mitochondrial Dysfunction in Obesity
Research increasingly suggests that obesity is associated with mitochondrial dysfunction in various tissues, including adipose tissue (fat tissue), skeletal muscle, and the liver. This dysfunction manifests in several ways:
- Reduced Mitochondrial Density and Size: Studies have shown that in obese individuals, the number and size of mitochondria in tissues like skeletal muscle and adipose tissue are often reduced. Fewer and smaller mitochondria translate to a lower capacity for energy production and fat oxidation.
- Impaired Oxidative Capacity: Even when present, mitochondria in obese individuals may exhibit a reduced ability to burn fat and produce ATP efficiently. This can lead to an accumulation of lipids within cells and contribute to insulin resistance, a common precursor to type 2 diabetes.
- Altered Mitochondrial Dynamics: Mitochondria are dynamic organelles that constantly undergo fusion (joining together) and fission (splitting apart) to maintain their health and function. In obesity, this balance can be disrupted, often leading to increased fragmentation of mitochondria. These smaller, fragmented mitochondria are often less efficient at energy production.
- Increased Reactive Oxygen Species (ROS) Production: Mitochondrial dysfunction can lead to increased production of harmful byproducts called reactive oxygen species (ROS). While some ROS are necessary for cellular signaling, excessive amounts can cause oxidative stress, damaging cellular components, including mitochondria themselves, further exacerbating the dysfunction.
How Obesity Impacts Mitochondria
The excess nutrients associated with a high-calorie diet, particularly a diet high in fat, can overwhelm the mitochondria. This nutrient overload can trigger a cascade of events leading to mitochondrial dysfunction:
- Lipid Overload: In adipose tissue, excessive fat intake leads to the accumulation of triglycerides within fat cells. This lipid overload can physically impair mitochondrial function and alter their structure.
- Inflammation: Obesity is characterized by chronic low-grade inflammation. Inflammatory molecules can directly interfere with mitochondrial function and contribute to their damage.
- Insulin Resistance: The impaired mitochondrial function in tissues like skeletal muscle can contribute to insulin resistance. When cells become resistant to insulin, glucose uptake is reduced, further disrupting energy metabolism and potentially exacerbating mitochondrial dysfunction.
- Specific Molecular Mechanisms: Recent research has identified specific molecules that play a role in the link between obesity and mitochondrial dysfunction. For example, a protein called RalA has been shown to be activated by a high-fat diet, leading to mitochondrial fragmentation and reduced fat burning in mice.
Consequences of Mitochondrial Dysfunction in Obesity
The vicious cycle of obesity and mitochondrial dysfunction can have significant consequences for overall health:
- Reduced Energy Expenditure: Impaired mitochondrial function can lead to a decrease in the body’s ability to burn calories, making weight loss more challenging and contributing to further weight gain.
- Metabolic Diseases: Mitochondrial dysfunction is strongly implicated in the development of metabolic diseases such as type 2 diabetes, non-alcoholic fatty liver disease (NAFLD), and cardiovascular disease.
- Systemic Inflammation: The increased ROS production and cellular stress resulting from mitochondrial dysfunction can contribute to systemic inflammation, further exacerbating obesity-related complications.
Potential Therapeutic Implications
Understanding the intricate relationship between mitochondria and obesity opens up potential avenues for therapeutic interventions. Strategies aimed at improving mitochondrial function could be beneficial in preventing and treating obesity and its associated metabolic complications. These strategies might include:
- Lifestyle Interventions: Exercise, particularly endurance training, has been shown to increase mitochondrial biogenesis and improve mitochondrial function in skeletal muscle. Caloric restriction can also positively impact mitochondrial health.
- Pharmacological Approaches: Researchers are exploring various pharmacological agents that can enhance mitochondrial function, reduce ROS production, and promote healthy mitochondrial dynamics.
- Nutritional Interventions: Certain nutrients and dietary components, such as antioxidants and specific fatty acids, may have a positive impact on mitochondrial function.
Conclusion
Mitochondria are far more than just cellular powerhouses; they are crucial regulators of energy balance. In the context of obesity, a complex interplay emerges where excess nutrient intake and inflammatory processes can impair mitochondrial function, leading to reduced energy expenditure, metabolic dysfunction, and a perpetuation of the obese state. Conversely, maintaining and improving mitochondrial health holds promise as a key strategy in combating obesity and its detrimental health consequences. Further research into the specific molecular mechanisms linking mitochondria and obesity will undoubtedly pave the way for more targeted and effective interventions.
Click Here to Buy Mitolyn Supplement to Help Fight Against Obesity!
Leave a Reply